Condition: Melasma

What is Melasma?
Melasma – also sometimes known as Chloasma or ‘Pregnancy Mask’ – is a relatively common skin concern. It is a condition which shows itself as darker patches of skin that occur usually on the face.
It is seen more in women than men, and is particularly common during pregnancy with approximately 50% of pregnant women experiencing the condition. It is non-cancerous, is more common in darker skin tones, and looks more prominent in the summer.
Melasma is particularly common in pregnant women due to the hormonal changes that occur during pregnancy. The excess production of hormones such as progesterone and oestrogen lead to increased melanin production, which causes dark patches to appear on the face of someone experiencing a melasma in pregnancy.
While melasma is a harmless condition that does not pose any major health risks, melasma on the face can cause psychological distress for those affected. As such, it is important, especially for pregnant women, to take necessary precautionary measures such as wearing a SPF daily of at least 30. It is advisable for pregnant women to avoid exposing their skin to direct sunlight as much as possible.
In addition, some medical conditions such as thyroid disease and Addison’s disease can also cause melasma. Therefore, it is important to consult with a healthcare professional if you notice any unusual changes in your skin.
What Causes Melasma?
Understanding the answer to “What is Melasma?” is essential to improving diagnosis and helping patients manage their condition effectively. Some causes of melasma include:
Hormonal changes:
Melasma is often triggered by hormonal changes in the body, such as pregnancy or the use of birth control pills. These changes can stimulate the production of melanocytes (pigment-producing cells) in the skin, leading to the development of melasma patches or melasma spots.
Sun exposure:
Excessive sun exposure is another major cause of melasma pigmentation. Ultraviolet (UV) rays from the sun can increase the production of melanin in the skin, leading to the development of dark patches on the skin and melasma sun damage on the face.
Genetics:
Some people are more prone to developing melasma due to genetic factors. If someone in your family has melasma skin, you may be at a higher risk of developing the condition.
Skin irritation:
Certain skincare products or cosmetic procedures can irritate the skin and trigger the development of melasma. Chemical peels, laser treatments, and harsh exfoliants could all possibly cause melasma pigmentation if your skin doesn’t react well to the treatment.
Medications:
Certain medications, such as antiepileptics, can lead to the development of melasma patches. This is because these drugs can stimulate the production of melanocytes in the skin.
Thyroid disorders:
People with thyroid disorders may be at a higher risk of developing melasma, as these disorders can affect the hormones responsible for the production of melanin in the skin. Additionally, Polycystic Ovary Syndrome (PCOS) can lead to hyperpigmentation melasma due to an overproduction of androgens. High levels of androgens can stimulate the melanocytes in the skin, causing them to produce excess pigment and PCOS melasma.
FAQ's
Is melasma different from hyperpigmentation?
Yes, melasma is different from hyperpigmentation, although they are often confused. Hyperpigmentation is a general term used to describe the darkening of skin due to an overproduction of melanin. This can be caused by a variety of factors such as sun exposure, hormonal changes, and inflammation.
Melasma, on the other hand, is a specific type of hyperpigmentation that is caused by hormonal factors, particularly oestrogen and progesterone.
How can I try and avoid getting melasma?
If you want to reduce your risk of developing melasma dark patches on face, it’s crucial to protect your skin from the sun. Melasma is often triggered by UV light, so wearing sunscreen with at least SPF 30 is essential – even in the winter.
Additionally, it is also recommended to avoid hormonal treatments, including birth control pills and hormone replacement therapy, which can increase your risk of developing hyperpigmentation melasma. Keeping your stress levels in check is another way to reduce your risk, as high levels of stress can also trigger melasma.
How can I get rid of melasma?
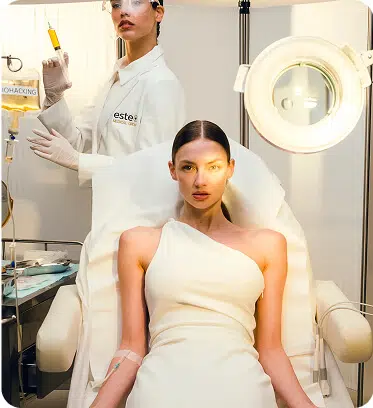
As of yet, there is no definitive treatment to remove melasma. However, here at Este Medical, we offer several clinically proven methods to effectively treat melasma skin, including melasma around mouth, melasma forehead, melasma on face, melasma on arms, melasma on back, and more.
Our safe and advanced melasma treatments including our Cosmelan Pigmentation Peel, HydraFacial, and Pixel Laser Resurfacing, are designed to give you the radiantly clear complexion you’ve been looking for. The medical professionals here at Este use only the latest technology and techniques to ensure the best possible outcome for you and your skin. Book your consultation today to get started on your journey to a newfound sense of confidence!
What is melasma?
Melasma is a common skin condition that causes brown or grey patches to appear on the face, particularly on the cheeks, chin, forehead, and nose. It mostly affects women and is often associated with pregnancy and hormonal changes. However, it can also develop in men and non-pregnant women due to sun exposure, genetics, and certain medications that increase the skin’s sensitivity to the sun.
How can I book my appointment?
Booking a consultation and appointment with us here at Este Medical Group is easy – simply enquire now and our specialists will be in touch with you shortly to arrange your visit.